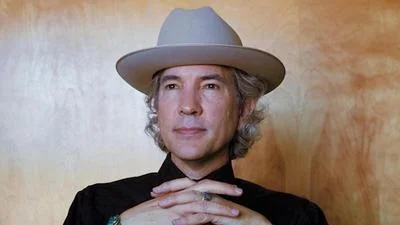
Douglas Ziedonis, MD, MPH, Executive Vice President for Health Sciences, CEO, UNM Health System | University Of New Mexico Health Sciences Center
The University of New Mexico College of Pharmacy and the UNM School of Medicine recently hosted a summit aimed at improving health care delivery across New Mexico. The “UNM P5 Summit” convened health care executives, providers, insurance companies, employers, and patients to explore innovative approaches and strengthen partnerships. Discussions focused on addressing health care needs and identifying future improvements.
Summit Goals and Key Outcomes
The summit highlighted New Mexico's pressing health care needs, particularly access and clinical gaps in care. With 32 out of 33 counties recognized as “Health Professional Shortage Areas,” fully utilizing the health care workforce is critical. Advanced Practice Pharmacists (APPh) were identified as pivotal in bridging these gaps. Key discussions included:
- Identifying health care access and clinical care gaps, especially in underserved areas.
- Describing current and future models for APPhs in New Mexico and other states.
- Integrating APPhs into team-based primary and specialty care settings.
- Developing innovative strategies for collaboration between patients and interprofessional health care teams.
- Creating and sustaining business models that support interprofessional health care teams.
Keynote and Panel Discussions
The summit featured keynote presentations on patient care gaps nationally and within New Mexico, setting the stage for panel discussions covering:
- Understanding what consumers need from the health care system.
- Reviewing various APPh models across the U.S. and their impact.
- Evaluating financial models and exploring enhanced partnerships.
Breakout Group Insights
Breakout sessions focused on identifying bridges and barriers to achieving the summit's goals. Key areas included:
- Addressing gaps in care through effective collaboration.
- Creating viable business models for team-based care.
- Improving communication within interprofessional teams.
- Developing training and protocols for expanding prescriptive authority.
The Prescription of Trust: Innovations in Health Care Roles
In a presentation titled "The Prescription of Trust," John McHugh, PhD, an assistant professor at Columbia University’s Mailman School of Public Health, discussed evolving dynamics within health care. Recent moves by corporate giants like CVS's acquisition of Oak Street Health and Amazon's purchase of One Medical signify a transformation toward population health management.
McHugh outlined three major pressures on the health care delivery system:
1. Value-Based Payment Models: Changing how care is paid for with a focus on cost outcomes. The value-based market could reach a trillion dollars in five years, but adoption among primary physicians remains limited.
2. Patient Complexity: Managing patients outside hospital settings is crucial, especially those over 65. Pharmacists play a significant role in reducing polypharmacy.
3. Primary Care Shortages: Projected shortages necessitate innovative solutions involving pharmacists' expanded roles.
Survey findings revealed high levels of trust in pharmacists' potential to manage medications for chronic conditions while technology reallocates resources allowing more direct patient interaction.
New Mexico Faces Significant Health Care Workforce Challenges
Michael Richards, MD, MPA, senior vice president for clinical affairs at UNM Health Sciences Center discussed severe workforce shortages exacerbated by socio-economic factors. Key issues impacting outcomes were outlined along with proposed solutions emphasizing social determinants such as community environment education economic stability personal behaviors reflecting significant challenges driving systemic interventions are necessary
Workforce Shortages
Although data suggests adequate numbers per capita access remains problematic particularly underserved areas Valencia County National benchmarks inadequately assess local needs
Tools Strategies Workforce Planning
HRSA provides tools projecting substantial shortages By 2035 require additional physicians nurses
Innovative Solutions Policy Changes
To mitigate shortages adopt innovative delivery models policy changes expanding allied professionals leveraging technology improving reimbursement Point-of-care testing treatment alleviate pressures
Health leaders advocate enhanced training programs creative distribution ensure statewide accessibility rural areas Collaborative practice agreements optimize resource utilization improve outcomes
ConclusionAddressing workforce challenges requires policy reform innovative models focus social determinants State's institutions produce professionals shape public policies drive necessary changes