The University of New Mexico Office for Community Health (OCH) has been awarded a five-year, $2.5 million federal grant to train primary care residents in Street Medicine. The training will take place at the Indian Health Service Family Medicine residency in Shiprock, New Mexico, as well as at the UNM Internal Medicine and Family Medicine residencies in Albuquerque.
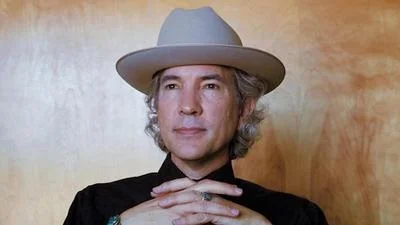
The funding comes from the Health Resources and Services Administration (HRSA), a federal agency that supports health care for people who are geographically isolated or vulnerable. According to Arthur Kaufman, MD, UNM’s vice president for Community Health, this initiative aims to address the medical needs of unhoused individuals who often do not have access to regular medical care.
“Residents will be out on the streets several times a week,” said Kaufman.
With this new grant, medical residents interested in focusing on Street Medicine will join mobile interdisciplinary teams. These teams include physicians, physician assistants, nurse practitioners, medical assistants, community health workers and Health Sciences students already involved in Street Medicine programs.
“They get to know where people stay, and they go out to visit them and keep medical records,” Kaufman explained. “They might be dressing a wound or making sure someone gets their diabetes medication.” He added that these teams can also provide mental health and substance use treatment directly on the street.
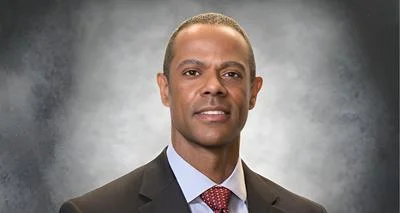
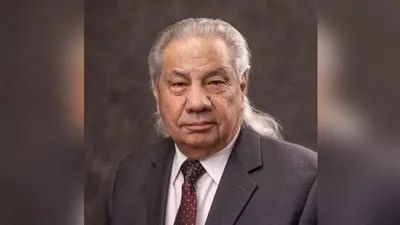
Janet Page-Reeves, PhD, director of OCH Research and vice chair of Research in UNM’s Department of Family & Community Medicine, developed the grant alongside Street Medicine leaders from both programs. These leaders include Asha Atwell, DO—an emergency physician at Northern Navajo Medical Center—and Sara Doorley, MD—an associate professor of Internal Medicine at UNM.
The Albuquerque Street Medicine program is officially called the Center for Inclusive Health Mobile Medical Team and is managed by the Division of General Internal Medicine within UNM School of Medicine’s Department of Internal Medicine. The HRSA grant will create collaboration with the Department of Family & Community Medicine so its residents can participate in this program.
Kaufman noted that the new funding will also support expansion of Atwell's Street Medicine program at Northern Navajo Medical Center under OCH supervision.
“Residents will be out on the streets several times a week,” Kaufman reiterated. By meeting people where they are located rather than expecting them to come into clinics or hospitals for treatment, providers hope to reach those unable or unwilling to visit traditional healthcare settings.
The Shiprock-UNM Family Medicine residency is currently the only Indian Health Service-based medical residency program in the United States; it was initially established with support from an earlier $2.5 million HRSA grant. This latest initiative builds upon previous work while adding further innovations through its focus on Street Medicine.